As your APP acclimates to clinical practice in your field, there will certainly be a lot to learn. Your department should offer the APP adequate educational resources to meet their needs -- lectures, articles, presentations, simulations, podcasts, outside courses, etc. More importantly, your department should help the APP sequence their efforts. For example, while knowing the proper work-up to identify a cause of stroke may be considered a foundational aspect of practicing within neurology, this may not be the most high-yield starting point for an APP being hired to work in the ALS multidisciplinary clinic. Viewing lectures on stroke syndrome or reading a review paper on secondary stroke prevention would therefore not be high yield activities to encourage your APP to pursue early in their training. Such topics can always be covered later, after the APP has settled into their clinical role. Early learning goals and didactic activities should instead match the APP’s early clinical priorities.
Develop a Knowledge Essentials List for Review with mentors, mapped to your EPAs
When planning for the clinical ramp-up of your APP, you determined the specific role your APP should play in your department and designed an outline of clinical priorities to be sequenced throughout their training period. As outlined above (link), some departments will choose to use patient logs to track key areas of clinical practice and inform the clinical complexity ramp-up. Other departments will specifically define and track those clinical with EPAs they design. In either case, creating a “schedule” of clinical priorities or EPAs is essential – this allows a department to easily structure out a formal onboarding curriculum.
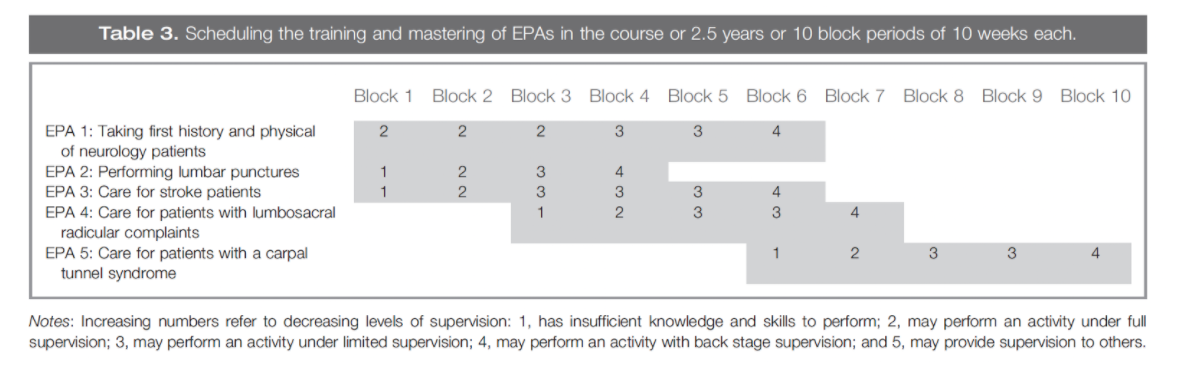
Consider the example above. During the first two blocks of this APP’s training, they could watch recorded lectures on physical exam techniques, have one-on-one sessions with their supervising MD to practice exam maneuvers, participate in a lumbar puncture skills session in the simulation center, and read a few review papers on stroke management. In block three, their didactics and readings could shift focus to lumbosacral radiculopathy. Educational objectives are easy to define in this model, and didactic learning is done in parallel with the real-time experiences the APP is having clinically.
Some departments will find it useful to designate a specific learning theme for each week. This creates a list of “Knowledge Essentials” that also allows the department to plan ahead and harmonize the APP’s educational activities—didactic lectures, mentored discussions, readings, etc. Early in the APP’s training, it can be especially useful to set aside 1-2 hours per week for free-form discussion with the supervising/collaborating MD and/or a senior APP in the department, focused on these key topics. The APP in training should be encouraged to bring specific questions or relevant cases they have seen to guide the discussions.
Distribute a Calendar of Departmental Conferences and Lectures
Begin by compiling a catalog of the existing education resources and events in your department. This helps emphasize the importance of shared responsibility in the training process of the APP. The goal should be to foster habits of self-directed independent study. The optimal role of the department is to ensure the APP has knowledge and access to all its resources; the optimal role of the APP is to determine which resources fit their needs best based on their current learning goals.
Educational resources to consider aggregating into your catalog:
-
Relevant hospital and departmental policies/clinical guidelines
-
Training Courses
-
STRATUS
-
Department held training courses
-
Certification courses i.e ACLS, ATLS
-
Grand Rounds calendar
-
M&M Conferences
-
Didactics/Conferences
-
Morning report
-
Residency curriculum schedule
-
Fellowship conferences
-
Divisional conferences
-
Bedside teaching rounds
-
Simulation opportunities
-
Journal subscriptions
-
Powerpoint libraries
-
Recorded Lectures and other Instructional Videos
Offer Additional Resources for Independent Study
Your APP will undoubtedly rely on resources outside of your department for their own independent study. Some useful resources will be obvious (e.g. UpToDate). Since your APP is just starting in your field, however, it can be very useful to help curate key resources. Consider providing recommendations in each of the following categories:
-
Textbooks
-
Choose one or two key works that emphasize the overall approach to patient care in your field. Remember factual knowledge is often more easily obtained through online resources or review papers
-
Journal Articles
-
Consider compiling a few key review papers and commonly cited clinical trials for common areas of clinical practice
-
Your department or residency program may already keep a shared folder of seminal papers in the field which you can draw from
-
Journals
-
Help your APP identify key subspecialty journals to keep an eye on for updates in your field
-
Podcasts
-
Specialty organizations or medical educators may host podcasts that offer a convenient, portable learning style that many learners prefer
-
Phone Apps
-
Do you use a visual acuity chart on your phone when examining patients? Your APP should probably have that, too
-
Conferences
-
Many specialty organizations now have APP-specific sessions at their annual meeting, or even an entirely separate conference. Help your APP identify useful continuing education opportunities.
-
Online modules or videos
-
If nothing comes to mind, ask the residents in your specialty’s program. They likely have identified useful resources for their own study.
